Treating Pain
October 19th, 2018
Treating Pain from a Biopsychosocial Perspective
Diane Belzil, RMT, CDT/MLD
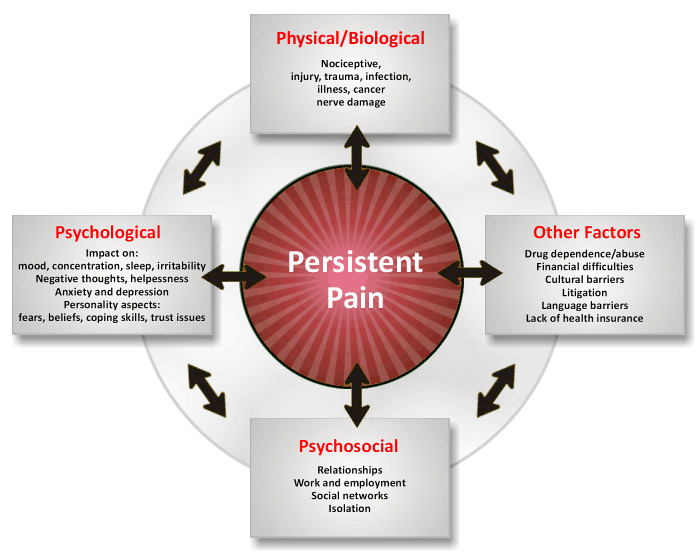
Pain is a tricky thing to understand, and in some ways the treatment of persistent pain (pain that continues for three months or more following an injury) has been moored to incorrect assumptions for decades. Luckily, it is becoming more and more common to find reference to the biopsychosocial model of pain, which takes into account how our psychological and social environment impacts our biology, and vica versa.
Keeping this model in mind allows the person in pain and their health care professionals to better understand why pain behaves the way that it does. Have you ever noticed that a painful spot on your body becomes more painful when you’re tired? What about when you’re stressed? Another, more subtle, example is that the pain associated with a motor vehicle accident often increases when the person returns to the site of the accident. All of these are examples of how our psychological and social environment impacts our biology—in these cases, by increasing the amount of pain experienced.
In my discussions with clients, I often hear them express the fear that their pain is not real, that they are imagining it or need to “just get over it.” Our culture is so heavily saturated with phrases like “no pain, no gain” and “mind over matter” that many of us assume that it is our own weakness that continues the pain cycle—that if we could simply “suck it up” the pain would go away.
Pain is always real and, though it may have begun at the time of an injury, it can continue beyond the presence of any tissue damage. This can be confusing and frightening for the person in pain, especially if they are told by health professionals that there is nothing wrong with them. As Lorimer Moseley and David Butler lay out in their excellent series Explain Pain, pain is a protective mechanism designed to prevent injury, and, just like any other mechanism in the human body, it can become overactive and thereby overprotective. In fact, to complicate matters even further, tissue damage can often be asymptomatic (meaning no pain is experienced!). Dr. Moseley neatly lays out this incredible phenomenon in a TedTalk he gave a few years ago.
Much of the current clinical approach to treating persistent pain involves the teasing out of pain from injury, and educating the public about the difference. Australia is currently at the forefront of this new approach, with programs like Tame the Beast and Pain Revolution offering practical, holistic approaches to the treatment of persistent pain for Australians.
Thankfully, the message is quickly spreading around the world, with more courses being offered for health professionals in Canada and more books like Explain Pain available for professionals and the public alike. I’ll be headed to Toronto this Fall for a course on this topic —stay tuned in the next newsletter for an update on what I’ve learned.
Posted in Health